What is Pelvic Health Physiotherapy?

Pelvic floor physiotherapy helps relieve pelvic pain and reduce symptoms of conditions caused by pelvic floor issues which include incontinence and painful intercourse. It is a specialized branch of physiotherapy involving internal and external assessment and treatment of the pelvic floor muscles. Those muscles are located between the hip bones and the sacrum, and they serve as a bowl to support the pelvic organs including the bladder, colon and uterus.
Pelvic Health Physio is covered under “physiotherapy” with most extended health insurance plans. Pelvic Physiotherapists have taken specialized courses that allow them to do an internal evaluation (although not always needed) to properly assess the pelvic floor muscles, nerves, ligaments and connective tissue.The goal of Pelvic Floor Physiotherapy is to improve pelvic floor function through exercises, lifestyle modifications, education and hands on treatment to decrease and eliminate your symptoms.
Doing Kegels is not always advisable! Kegels are not for everyone, and even when indicated are often not done properly! If you have been told to do Kegels and find you are getting worse, or are not sure if you are doing them correctly, book an appointment to make sure you are doing the right thing! We will consider you as a whole person and customize treatments to address your issues unique to you.
Benefits of pelvic floor physiotherapy?
You may benefit from pelvic floor physiotherapy if you have any type of pelvic floor dysfunction. Pelvic floor dysfunction can be classified into two problems: your muscles are too tight or they are too weak.
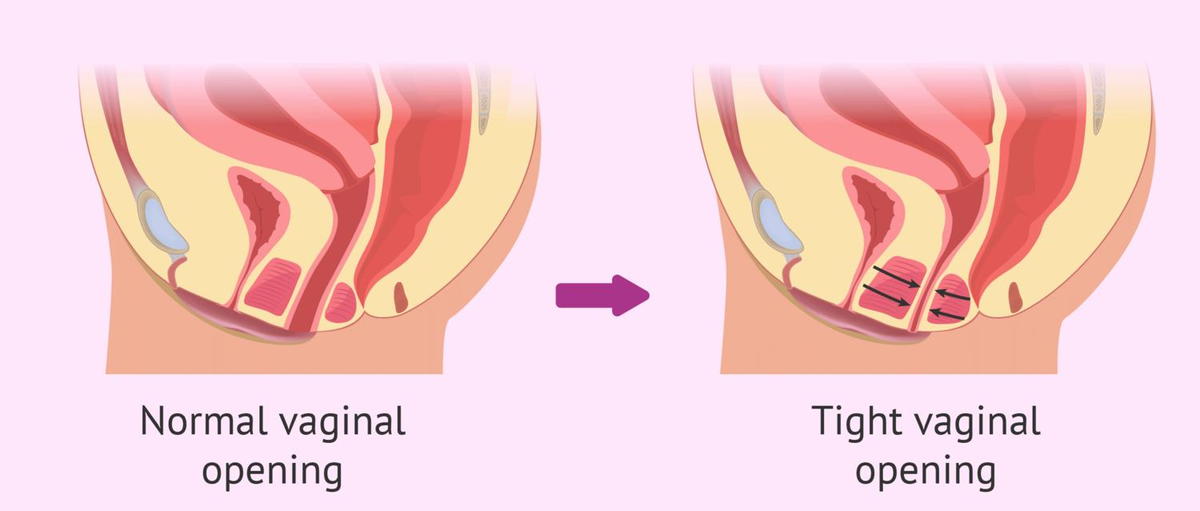
Hypertonic (Tight pelvic floor muscles) can cause the following symptoms:
Urinary frequency, urgency, hesitancy, stopping and starting of the urine stream, painful urination, or incomplete emptying, waking up during the night with a need to pee.
Constipation, straining, pain with bowel movements
Unexplained pain in your low back, pelvic region, hips, genital area, or rectum
If you suffer from a tight, dysfunctional pelvic floor, you may also experience sexual dysfunction. This can present as pain with penetration, inability to have vaginal penetration, pain with or inability to orgasm, and pain with sexual stimulation. In men, it can also present as painful erections and premature ejaculation.
Uncoordinated muscle contractions causing the pelvic floor muscles to spasm
Hypotonicity (Weak pelvic floor muscles) can cause the following symptoms
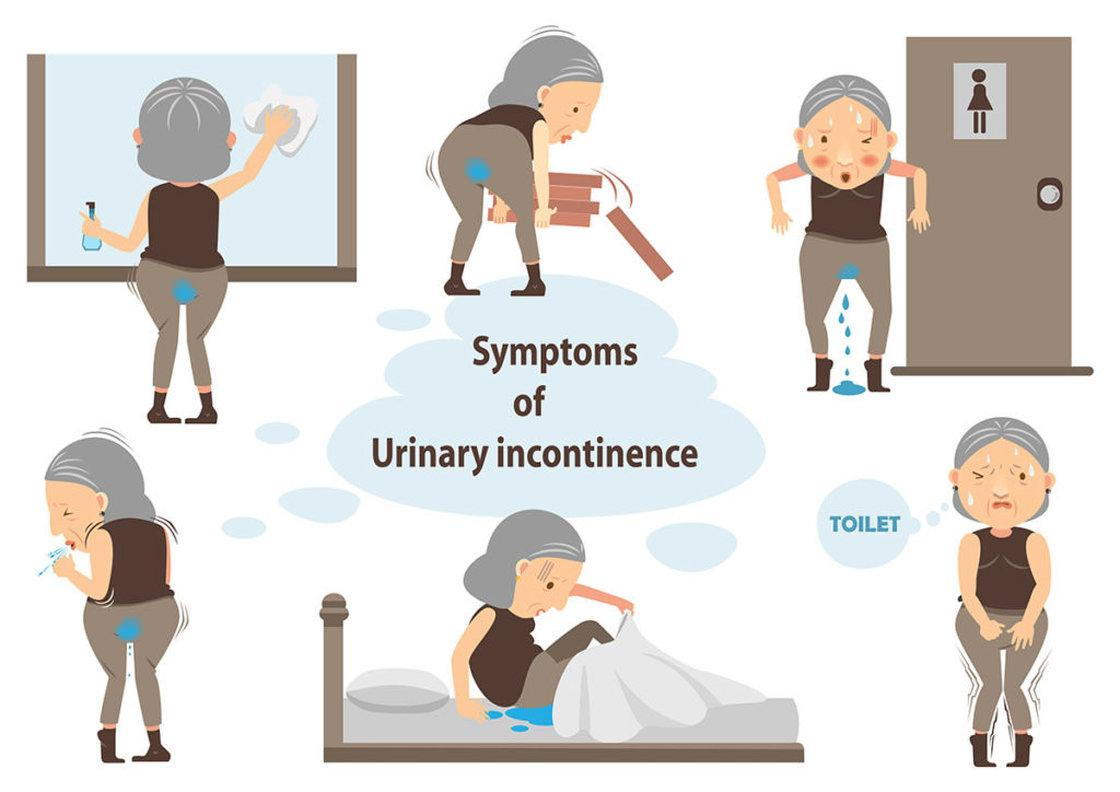
urge incontinence
stress incontinence, which is the involuntary loss of urine or stool during or after activity. This includes leaking during sports, or with coughing and sneezing.
pelvic organ prolapse.which is when one of the pelvic organs starts to shift out of place. This contributes to heaviness or bulging at the vaginal or rectal opening.These are conditions typically associated with women after they give birth, and as a result, most women think this is a normal turn of events and do not realize this is something that can be fixed! The good news is, there is a solution beyond pads and diapers.
Incontinence is NOT a normal part of aging
Common Conditions treated with pelvic floor physiotherapy
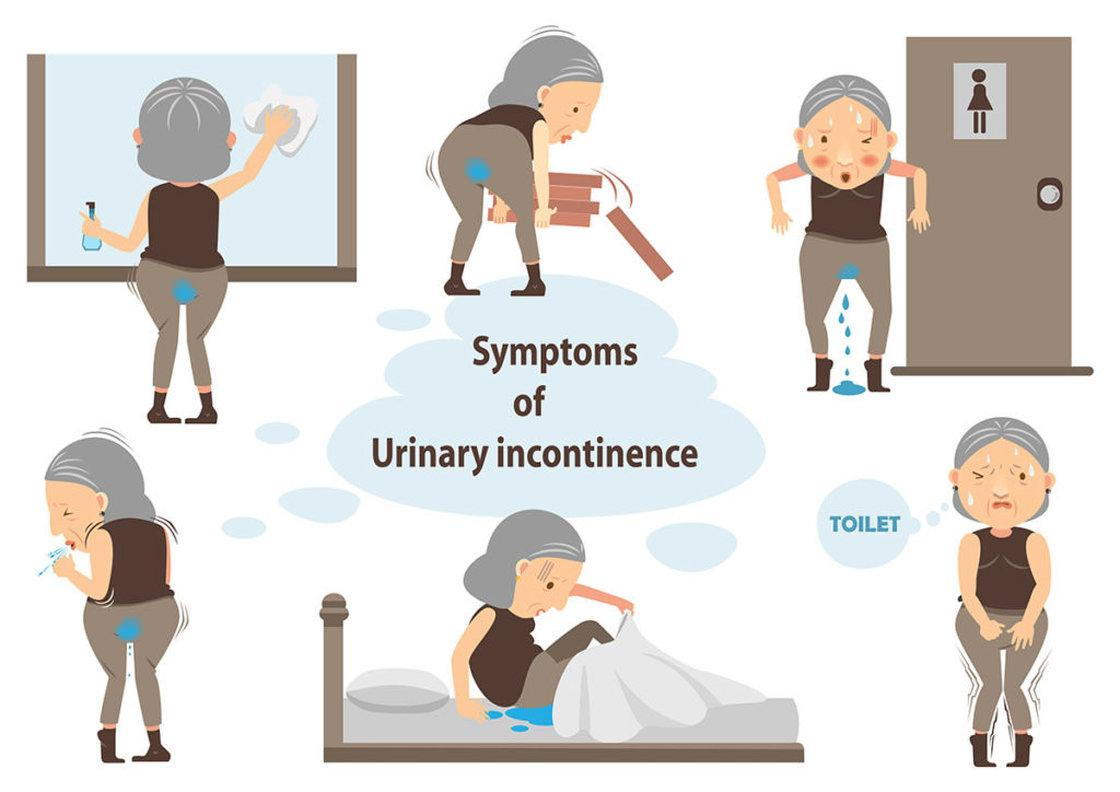
Incontinence
Incontinence is the uncontrolled loss of urine, gas or stool in any amount. Urinary incontinence may occur due to activities that increase pressures in the abdominal canister and on the bladder – such as running, coughing, jumping, lifting or laughing. This is called stress urinary incontinence and is the most common form of incontinence that we see.
Incontinence may also result from a strong and sudden urge to void. If that strong urge cannot be controlled, then a leak occurs. This type of leaking is called urge urinary incontinence. Other types of incontinence exist as well.
Mixed incontinence which is urine loss associated with increases in intra-abdominal pressure (stress incontinence) and with an intense urge to void (urge incontinence).
Overflow incontinence in which the bladder doesn’t empty normally and becomes very full (distended bladder) and there is constant loss of small amount of urine (dribbles)
Functional incontinence is urinary leakage which is associated with impairment of cognitive or physical function (broken hip), psychological unwillingness or environmental barriers to the toilet
Although urinary incontinence may be common, it is not normal and can be effectively treated by pelvic floor physiotherapy.
Pelvic organ prolapse
It is a subjective disorder described as an annoying protrusion (bulge) at or near the vaginal opening, which may or may not be accompanied by perineal pressure (pressure between your vagina and anus) Positions where gravity is acting on the body (such as standing, walking, lifting) tend to aggravate signs and symptoms. And positions where gravity is not a factor (such as lying down) tend to be relieving.
Prolapse is described by the organ which is protruding into the vaginal canal. They include:
Cystocele: Prolapse of the bladder
Rectocele: Prolpase of the rectum
Urethrocele: Prolapse of the urethra
Uterine prolapse: Prolapse of the uterus
Vaginal Vault prolapse: Prolapse of the top of the vagina after a hysterectomy
Enterocele: Prolapse of the intestines
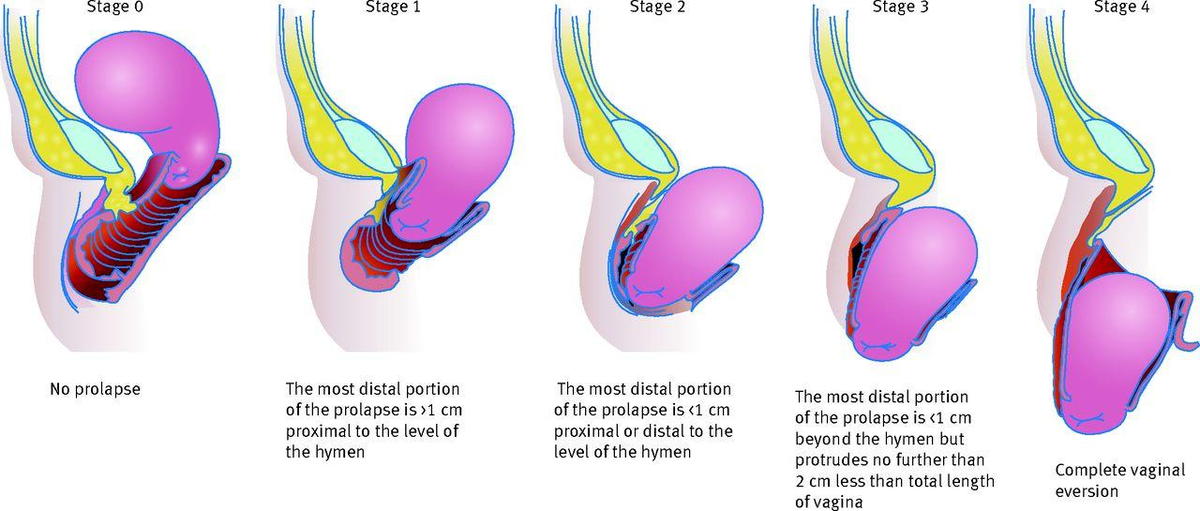
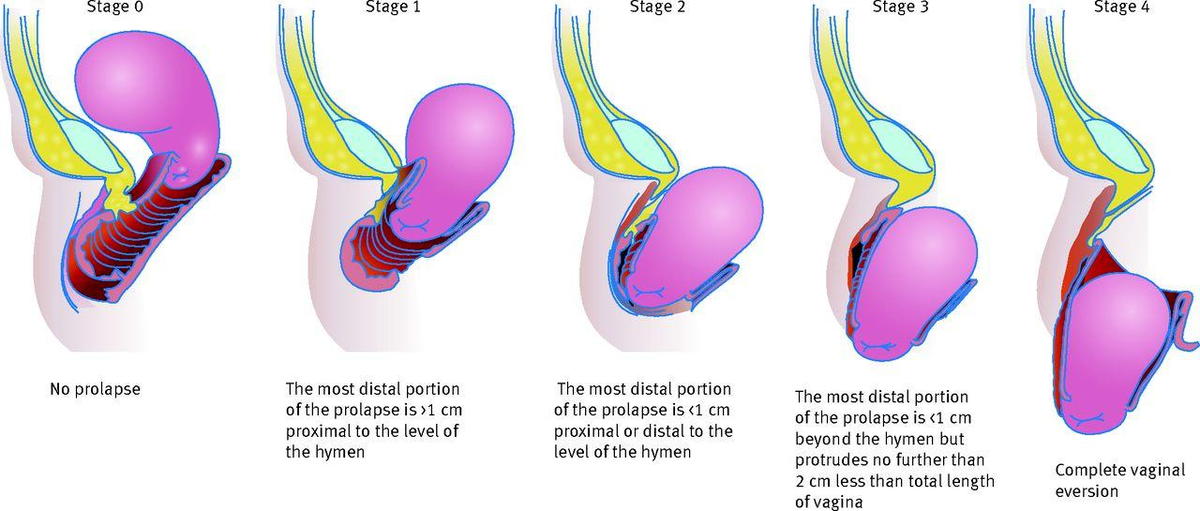
There are a few different ways to measure or grade a prolapse. One of the most widely used staging systems is the POP-Q (Pelvic Organ Prolapse Quantification System). It uses a four point system to determine the degree of prolapse that someone has.
Stage 0 = no prolapse
Stage 1 = prolapse is at 1cm above the vaginal opening or higher
Stage 2 = prolapse is 1cm away from vaginal opening or has protruded up to 1cm out of the vagina
Stage 3 = prolapse protrudes more than 1cm out of the vagina but no more than 2cm
Stage 4 = vaginal walls have completed everted and prolapse has maximally protruded
Pelvic floor physiotherapy is very effective at treating prolapses in stages 1 to 3 using the POP-Q.
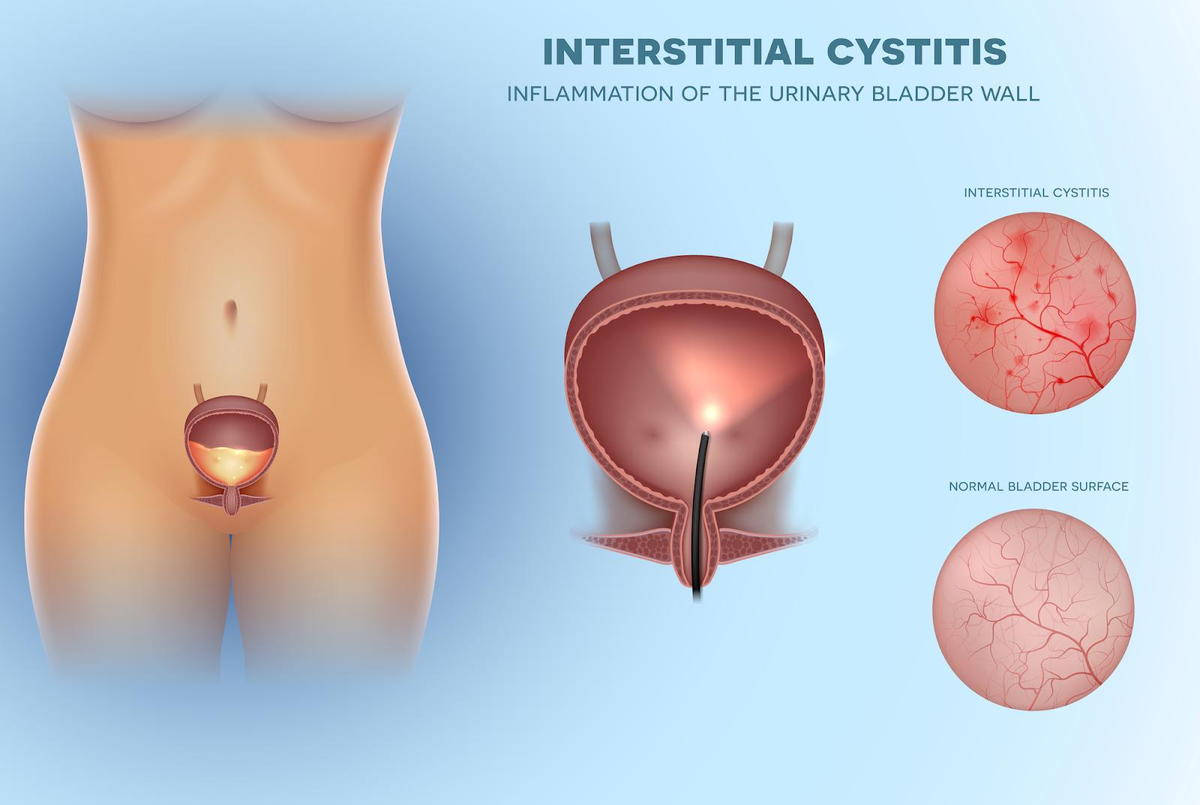
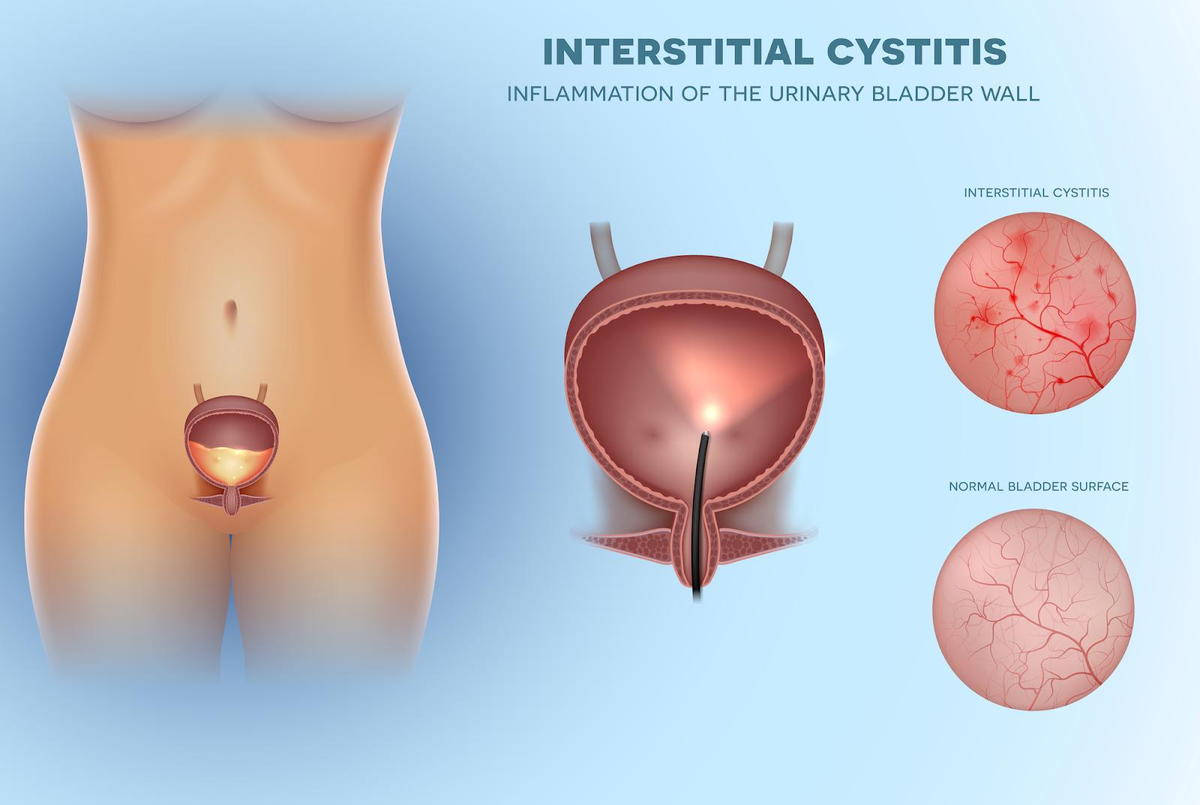
Interstitial Cystitis
Interstitial cystitis/painful bladder syndrome is defined as “an unpleasant sensation (pain, pressure and discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes”. Although it has traditionally been looked at as a problem of the bladder and treatment protocols in traditional medical approaches have focussed on treating the bladder, it has been reported in a study that women who were diagnosed with IC reported pain in the pelvic muscles (their typical pain was felt in the bladder when the muscles were palpated) and not in the bladder when the bladder was palpated.
So is it the pelvic floor causing bladder pain? Or the bladder causing pelvic floor dysfunction? That is what research is working on figuring out.
But for our purposes, it doesn’t really matter. We know that when we work directly on the pelvic floor tissues, we can impact the state of the bladder as well.
Our pelvic floor work involves improving tissue health, flexibility and range of motion, compliance, texture, tone, position, resilience, coordination and more.
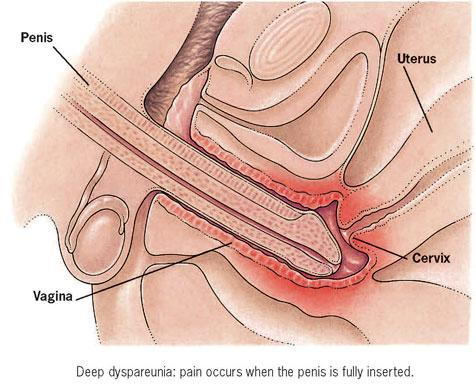
Dyspareunia
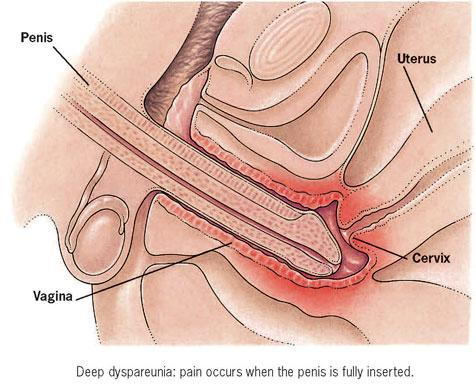
Dyspareunia, or pain associated with intercourse, can be experienced during penetration, with thrusting, or both. It can also be used to describe the pain felt after intercourse, which may or may not be accompanied by pain during intercourse. Pain with penetration is usually described as very sharp with burning, ripping or tearing sensations. The pain with thrusting can be sharp, or dull and achy. Deep dyspareunia on thrusting can also be described as putting pressure on a tender bruise. Pain after intercourse will often be described as an intense aching or soreness, sometimes with severe burning and occasional sharp stabs of pain.Many factors can contribute to the development of pain during sex. They include:
viral, bacterial, or fungal infections
Connective tissue dysfunction
pelvic organ prolapse
vaginal dryness and irritation
vulvar skin changes
hormonal changes during pregnancy, postpartum, or perimenopause
oral contraceptives
episiotomy
hypertonicity in pelvic floor muscles
chemicals in personal care products (eg. lube, soaps, condoms etc)
allergic reactions
female genital cutting
labial micro tears
vulvovaginal and anal fissures
pudendal nerve irritation or pelvic nerve compression
restrictive scar tissue
pelvic or abdominal surgeries
central nervous system sensitization
a combination of any of the above
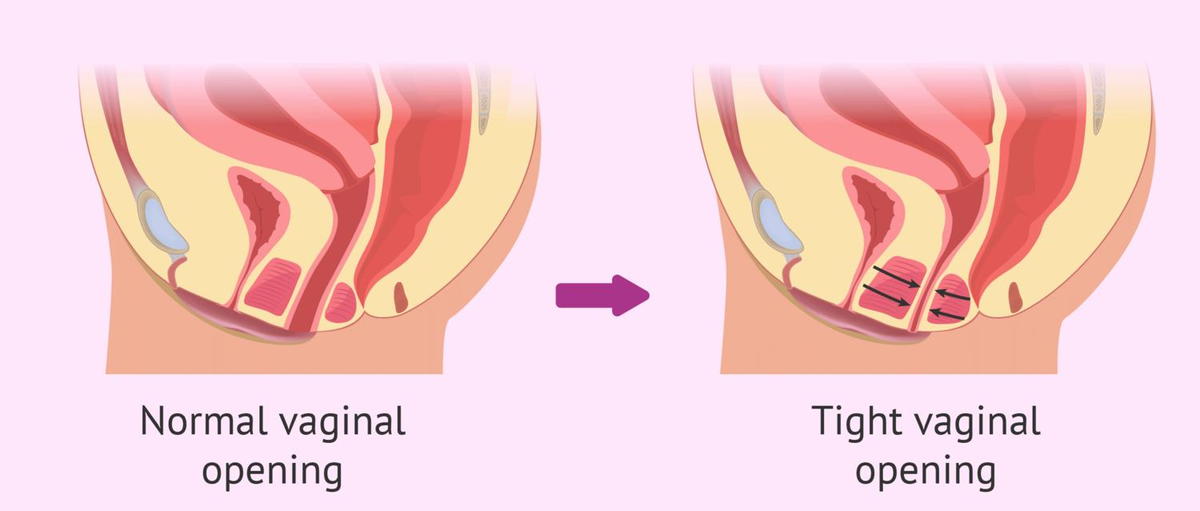
Vaginismus
Vaginismus is the inability to have penetration into the vagina with a penis, finger or tampon.Vaginismus can be classified as primary (where penetration has never been possible), or secondary (where penetration was possible at one point but is no longer possible). With Vaginismus, there is usually significant Connective Tissue Dysfunction that needs to be addressed first before internal work is completed
Pelvic floor physiotherapy helps women with vaginismus overcome pain and muscle spasm by:
Improving position, texture, range of motion, elasticity, tone, mobility, and function of pelvic floor muscles, connective tissue, and myofascia.
Down-regulating the sensitive nervous system, remapping the brain, and retraining the system from a top down approach.
Providing education and training on how to use products such as dilators, therapy wands, lube, and more.
Providing education on sex and sexuality in relation to pelvic health and rehabilitation.
Vulvodynia
Vulvodynia is a broad category of pelvic pain that can be broken down into smaller subset diagnoses. They include:
Vestibulodynia (pain at the vestibule or “entrance” of the vagina)
Vulvodynia (pain in the superficial tissues of the vulva, particularly the labia majora and minora)
Clitordynia (pain at the clitoris)
Vulvodynia is a diagnosis of exclusion. This means that the diagnosis of vulvodynia is given only after all other possible causes of vulvar pain have been ruled out. Although no one knows exactly what causes vulvodynia, there are a number of factors that are associated with it:
Hormonal factors
Inflammatory factors
Nutritional factors
Genetic factors
Nervous system factors
Orthopaedic factors
Nervous system factors
Psychological and social factors
Pelvic floor muscle overactivity
Presence of other pain syndromes
With pelvic floor physiotherapy, we treat your vulva, your pelvic floor, and your pain system. We provide you with various tools and strategies to manage, reduce, and overcome your pain.
Most importantly we adopt a biopsychosocial approach to care. This means we look at you as a whole person, not just one part. We consider the physical, emotional, psychological, and spiritual factors that may be impacting your health, wellness, and experience with pain. We understand the psycho-somatic nature of pain – that the body impacts the brain and the brain impacts the body.
Dysmenorrhea
Dysmenorrhea is the medical term used to describe pain before or during menstrual periods. Symptoms of dysmenorrhea can begin immediately following ovulation (mid-cycle) and can last until the end of menstruation (end of your bleed)
Symptoms typically last less than three days. The pain is usually in the pelvis or lower abdomen. Other symptoms may include lower back pain, pain that radiates to the thighs, diarrhea, or nausea.
Dysmenorrhea occurs less often in those who exercise regularly and those who have children early in life.
Seeing a physiotherapist can help with the symptoms of dysmenorrhea. Expect your physiotherapist to assess the muscles and connective tissues of your abdomen, pelvic girdle and pelvic floor. Your physiotherapist can teach you how to relax these muscles, use deep breathing and other relaxation strategies, and help you with stress management.
Pelvic floor Physiotherapy treatment
Every treatment is tailored to your individual needs as a client. There is an external examination component where the skin, fascia, and muscles of the abdomen, lower back, and inner thighs are assessed. There is also an internal component to the exam which is done via a digital (finger) vaginal and/or rectal exam.
An internal exam is not always necessary, but it is encouraged to get a full picture of the issues you may have. It also adds valuable insight to better enhance your treatment plan and reach the best outcomes possible, in the shortest amount of time.
Pelvic floor physiotherapists help women rehabilitate their pelvic floor muscles. These muscles can be weakened by childbirth, surgery, heavy lifting, being overweight, constipation or menopause. The pelvic floor muscles support the womb (uterus), bladder and bowel (colon), forming a 'sling' from the pubic bone at the front to the tailbone at the back. If the muscles are weak, this can affect bladder and bowel control, resulting in incontinence (leakage) or prolapse.
For other women, their pelvic floor muscles may be overactive; that is, they can switch on involuntarily when they should be relaxing. These women need to learn to release their muscles. Overactivity can cause difficulty with having sex, emptying the bladder or bowels or using tampons.
This could include exercises, biofeedback (electronic monitoring), and manual treatment of the muscles. Advice about daily activities and fitness, as well as good bladder and bowel habits, will be given. Functional training of the pelvic floor gets your muscles back working effectively when you need them.
A pelvic floor physiotherapist is an important part of the multi-disciplinary team managing bladder and bowel health, sexual difficulties and pelvic pain.

Pelvic floor physiotherapy helps relieve pelvic pain and reduce symptoms of conditions caused by pelvic floor issues which include incontinence and painful intercourse. It is a specialized branch of physiotherapy involving internal and external assessment and treatment of the pelvic floor muscles. Those muscles are located between the hip bones and the sacrum, and they serve as a bowl to support the pelvic organs including the bladder, colon and uterus.
Pelvic Health Physio is covered under “physiotherapy” with most extended health insurance plans. Pelvic Physiotherapists have taken specialized courses that allow them to do an internal evaluation (although not always needed) to properly assess the pelvic floor muscles, nerves, ligaments and connective tissue.The goal of Pelvic Floor Physiotherapy is to improve pelvic floor function through exercises, lifestyle modifications, education and hands on treatment to decrease and eliminate your symptoms.
Doing Kegels is not always advisable! Kegels are not for everyone, and even when indicated are often not done properly! If you have been told to do Kegels and find you are getting worse, or are not sure if you are doing them correctly, book an appointment to make sure you are doing the right thing! We will consider you as a whole person and customize treatments to address your issues unique to you.
Benefits of pelvic floor physiotherapy?
You may benefit from pelvic floor physiotherapy if you have any type of pelvic floor dysfunction. Pelvic floor dysfunction can be classified into two problems: your muscles are too tight or they are too weak.
Hypertonic (Tight pelvic floor muscles) can cause the following symptoms:
Urinary frequency, urgency, hesitancy, stopping and starting of the urine stream, painful urination, or incomplete emptying, waking up during the night with a need to pee.
Constipation, straining, pain with bowel movements
Unexplained pain in your low back, pelvic region, hips, genital area, or rectum
If you suffer from a tight, dysfunctional pelvic floor, you may also experience sexual dysfunction. This can present as pain with penetration, inability to have vaginal penetration, pain with or inability to orgasm, and pain with sexual stimulation. In men, it can also present as painful erections and premature ejaculation.
Uncoordinated muscle contractions causing the pelvic floor muscles to spasm
Hypotonicity (Weak pelvic floor muscles) can cause the following symptoms
urge incontinence
stress incontinence, which is the involuntary loss of urine or stool during or after activity. This includes leaking during sports, or with coughing and sneezing.
pelvic organ prolapse.which is when one of the pelvic organs starts to shift out of place. This contributes to heaviness or bulging at the vaginal or rectal opening.These are conditions typically associated with women after they give birth, and as a result, most women think this is a normal turn of events and do not realize this is something that can be fixed! The good news is, there is a solution beyond pads and diapers.
Incontinence is NOT a normal part of aging
Common Conditions treated with pelvic floor physiotherapy
Incontinence
Incontinence is the uncontrolled loss of urine, gas or stool in any amount. Urinary incontinence may occur due to activities that increase pressures in the abdominal canister and on the bladder – such as running, coughing, jumping, lifting or laughing. This is called stress urinary incontinence and is the most common form of incontinence that we see.
Incontinence may also result from a strong and sudden urge to void. If that strong urge cannot be controlled, then a leak occurs. This type of leaking is called urge urinary incontinence. Other types of incontinence exist as well.
Mixed incontinence which is urine loss associated with increases in intra-abdominal pressure (stress incontinence) and with an intense urge to void (urge incontinence).
Overflow incontinence in which the bladder doesn’t empty normally and becomes very full (distended bladder) and there is constant loss of small amount of urine (dribbles)
Functional incontinence is urinary leakage which is associated with impairment of cognitive or physical function (broken hip), psychological unwillingness or environmental barriers to the toilet
Although urinary incontinence may be common, it is not normal and can be effectively treated by pelvic floor physiotherapy.
Pelvic organ prolapse
It is a subjective disorder described as an annoying protrusion (bulge) at or near the vaginal opening, which may or may not be accompanied by perineal pressure (pressure between your vagina and anus) Positions where gravity is acting on the body (such as standing, walking, lifting) tend to aggravate signs and symptoms. And positions where gravity is not a factor (such as lying down) tend to be relieving.
Prolapse is described by the organ which is protruding into the vaginal canal. They include:
Cystocele: Prolapse of the bladder
Rectocele: Prolpase of the rectum
Urethrocele: Prolapse of the urethra
Uterine prolapse: Prolapse of the uterus
Vaginal Vault prolapse: Prolapse of the top of the vagina after a hysterectomy
Enterocele: Prolapse of the intestines
There are a few different ways to measure or grade a prolapse. One of the most widely used staging systems is the POP-Q (Pelvic Organ Prolapse Quantification System). It uses a four point system to determine the degree of prolapse that someone has.
Stage 0 = no prolapse
Stage 1 = prolapse is at 1cm above the vaginal opening or higher
Stage 2 = prolapse is 1cm away from vaginal opening or has protruded up to 1cm out of the vagina
Stage 3 = prolapse protrudes more than 1cm out of the vagina but no more than 2cm
Stage 4 = vaginal walls have completed everted and prolapse has maximally protruded
Pelvic floor physiotherapy is very effective at treating prolapses in stages 1 to 3 using the POP-Q.
Interstitial Cystitis
Interstitial cystitis/painful bladder syndrome is defined as “an unpleasant sensation (pain, pressure and discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than six weeks duration, in the absence of infection or other identifiable causes”. Although it has traditionally been looked at as a problem of the bladder and treatment protocols in traditional medical approaches have focussed on treating the bladder, it has been reported in a study that women who were diagnosed with IC reported pain in the pelvic muscles (their typical pain was felt in the bladder when the muscles were palpated) and not in the bladder when the bladder was palpated.
So is it the pelvic floor causing bladder pain? Or the bladder causing pelvic floor dysfunction? That is what research is working on figuring out.
But for our purposes, it doesn’t really matter. We know that when we work directly on the pelvic floor tissues, we can impact the state of the bladder as well.
Our pelvic floor work involves improving tissue health, flexibility and range of motion, compliance, texture, tone, position, resilience, coordination and more.
Dyspareunia
Dyspareunia, or pain associated with intercourse, can be experienced during penetration, with thrusting, or both. It can also be used to describe the pain felt after intercourse, which may or may not be accompanied by pain during intercourse. Pain with penetration is usually described as very sharp with burning, ripping or tearing sensations. The pain with thrusting can be sharp, or dull and achy. Deep dyspareunia on thrusting can also be described as putting pressure on a tender bruise. Pain after intercourse will often be described as an intense aching or soreness, sometimes with severe burning and occasional sharp stabs of pain.Many factors can contribute to the development of pain during sex. They include:
viral, bacterial, or fungal infections
Connective tissue dysfunction
pelvic organ prolapse
vaginal dryness and irritation
vulvar skin changes
hormonal changes during pregnancy, postpartum, or perimenopause
oral contraceptives
episiotomy
hypertonicity in pelvic floor muscles
chemicals in personal care products (eg. lube, soaps, condoms etc)
allergic reactions
female genital cutting
labial micro tears
vulvovaginal and anal fissures
pudendal nerve irritation or pelvic nerve compression
restrictive scar tissue
pelvic or abdominal surgeries
central nervous system sensitization
a combination of any of the above
Vaginismus
Vaginismus is the inability to have penetration into the vagina with a penis, finger or tampon.Vaginismus can be classified as primary (where penetration has never been possible), or secondary (where penetration was possible at one point but is no longer possible). With Vaginismus, there is usually significant Connective Tissue Dysfunction that needs to be addressed first before internal work is completed
Pelvic floor physiotherapy helps women with vaginismus overcome pain and muscle spasm by:
Improving position, texture, range of motion, elasticity, tone, mobility, and function of pelvic floor muscles, connective tissue, and myofascia.
Down-regulating the sensitive nervous system, remapping the brain, and retraining the system from a top down approach.
Providing education and training on how to use products such as dilators, therapy wands, lube, and more.
Providing education on sex and sexuality in relation to pelvic health and rehabilitation.
Vulvodynia
Vulvodynia is a broad category of pelvic pain that can be broken down into smaller subset diagnoses. They include:
Vestibulodynia (pain at the vestibule or “entrance” of the vagina)
Vulvodynia (pain in the superficial tissues of the vulva, particularly the labia majora and minora)
Clitordynia (pain at the clitoris)
Vulvodynia is a diagnosis of exclusion. This means that the diagnosis of vulvodynia is given only after all other possible causes of vulvar pain have been ruled out. Although no one knows exactly what causes vulvodynia, there are a number of factors that are associated with it:
Hormonal factors
Inflammatory factors
Nutritional factors
Genetic factors
Nervous system factors
Orthopaedic factors
Nervous system factors
Psychological and social factors
Pelvic floor muscle overactivity
Presence of other pain syndromes
With pelvic floor physiotherapy, we treat your vulva, your pelvic floor, and your pain system. We provide you with various tools and strategies to manage, reduce, and overcome your pain.
Most importantly we adopt a biopsychosocial approach to care. This means we look at you as a whole person, not just one part. We consider the physical, emotional, psychological, and spiritual factors that may be impacting your health, wellness, and experience with pain. We understand the psycho-somatic nature of pain – that the body impacts the brain and the brain impacts the body.
Dysmenorrhea
Dysmenorrhea is the medical term used to describe pain before or during menstrual periods. Symptoms of dysmenorrhea can begin immediately following ovulation (mid-cycle) and can last until the end of menstruation (end of your bleed)
Symptoms typically last less than three days. The pain is usually in the pelvis or lower abdomen. Other symptoms may include lower back pain, pain that radiates to the thighs, diarrhea, or nausea.
Dysmenorrhea occurs less often in those who exercise regularly and those who have children early in life.
Seeing a physiotherapist can help with the symptoms of dysmenorrhea. Expect your physiotherapist to assess the muscles and connective tissues of your abdomen, pelvic girdle and pelvic floor. Your physiotherapist can teach you how to relax these muscles, use deep breathing and other relaxation strategies, and help you with stress management.
Pelvic floor Physiotherapy treatment
Every treatment is tailored to your individual needs as a client. There is an external examination component where the skin, fascia, and muscles of the abdomen, lower back, and inner thighs are assessed. There is also an internal component to the exam which is done via a digital (finger) vaginal and/or rectal exam.
An internal exam is not always necessary, but it is encouraged to get a full picture of the issues you may have. It also adds valuable insight to better enhance your treatment plan and reach the best outcomes possible, in the shortest amount of time.
Pelvic floor physiotherapists help women rehabilitate their pelvic floor muscles. These muscles can be weakened by childbirth, surgery, heavy lifting, being overweight, constipation or menopause. The pelvic floor muscles support the womb (uterus), bladder and bowel (colon), forming a 'sling' from the pubic bone at the front to the tailbone at the back. If the muscles are weak, this can affect bladder and bowel control, resulting in incontinence (leakage) or prolapse.
For other women, their pelvic floor muscles may be overactive; that is, they can switch on involuntarily when they should be relaxing. These women need to learn to release their muscles. Overactivity can cause difficulty with having sex, emptying the bladder or bowels or using tampons.
This could include exercises, biofeedback (electronic monitoring), and manual treatment of the muscles. Advice about daily activities and fitness, as well as good bladder and bowel habits, will be given. Functional training of the pelvic floor gets your muscles back working effectively when you need them.
A pelvic floor physiotherapist is an important part of the multi-disciplinary team managing bladder and bowel health, sexual difficulties and pelvic pain.
Visit our Office
Peak Rehab
2 Kennedy Rd S Suite #4A
Brampton, ON L6W 3E1, Canada
